Erythropoietic Protoporphyria (EPP)
About EPP
EPP is a rare metabolic disorder that causes severe, or phototoxic, reactions to light and affects approximately 10,000 people globally.
Patients with EPP have a deficiency of ferrochelatase, an enzyme which is involved in the formation of haemoglobin. This deficiency causes a precursor chemical called protoporphyrin IX to accumulate in the body and skin. Protoporphyrin IX is highly reactive with sunlight, resulting in severe inflammation and pain after only a few minutes of sun exposure.
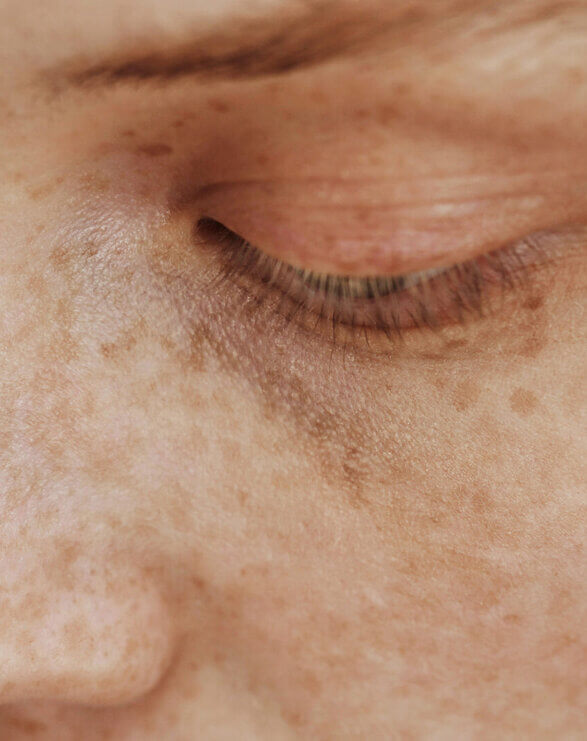
EPP symptoms can occur suddenly (acute), or delayed (subacute), and are most often expressed as intense burning, tingling and itching of sun-exposed skin, followed by redness and swelling. Long-term exposure to light can cause scarring.
Phototoxicity is unresponsive to traditional pain and burn management techniques and patients can be incapacitated for days before reactions subside. Most patients must withdraw from light exposure in order to manage their symptoms.
Children and adults living with EPP must avoid sunlight and even reflected light for life, often staying indoors or wearing protective clothing. Conventional sunscreens have little to no effect as they do not block the wavelengths of light which cause phototoxicity in EPP.
What is Erythropoietic Protoporphyria?
Learn more about EPP.
EPP Clinical Results
November 2013
CLINUVEL announced results from its US Phase III study of SCENESSE® (afamelanotide 16mg) (CUV039).
November 2011
CLINUVEL announced results from its first US Phase II study of SCENESSE® (afamelanotide 16mg) (CUV030).
July 2010
CLINUVEL released full report from the CUV017 study.
December 2009
CLINUVEL announced preliminary results from its lead Phase III study of SCENESSE® in 100 patients diagnosed with EPP (CUV017).
January 2009
CLINUVEL announced interim results from its lead Phase III study of SCENESSE® (afamelanotide 16mg) in patients diagnosed with EPP (CUV017). The data from the first 14 Swiss patients to complete the 12 month study period were analysed, showing SCENESSE® was of clinical benefit in EPP.
Clinical & regulatory progress
Future
CLINUVEL is working to facilitate access to EPP patients in a number of countries. For more specific info, please contact us.
February 2025
CLINUVEL announced preliminary results from its post-authorisation study of SCENESSE® (afamelanotide) in adult and adolescent (12–17-year-old) erythropoietic protoporphyria (EPP) patients (CUV052).
Pending final analyses, data from the CUV052 study will form part of the regulatory package to be submitted to regulatory agencies in support of expanding the SCENESSE® indication to include treatment of adolescent patients.Read the announcement.
September 2023
CLINUVEL shared a regulatory update on the European label expansion of SCENESSE® (afamelanotide 16mg) to facilitate treatment of adolescent (12‒17 years old) erythropoietic protoporphyria (EPP) patients. Read the announcement.
July 2023
CLINUVEL announced that it has been awarded a five-year contract by the U.S. Department of Veterans Affairs (VA) to supply SCENESSE® (afamelanotide) for adult erythropoietic protoporphyria (EPP) patients. The listings enable any adult EPP patient covered by the VA health care program to receive SCENESSE® treatment at all VA facilities until July 2028, when the contract can be reviewed and renewed. Read the announcement.
May 2023
CLINUVEL announced that the first Canadian EPP patient has received treatment under a Special Access Program (SAP) approved by Health Canada. Read the announcement for more details.
September 2022
CLINUVEL submitted a variation to its marketing authorisation dossier for SCENESSE® to the EMA, providing scientific data supporting the expansion of the authorised indication to include adolescent patients aged 12 years and older. In parallel, the Company has updated its paediatric investigation plan for SCENESSE® to reflect the proposed label expansion. Read the announcement.
February 2021
Market access granted in Israel.
October 2020
SCENESSE® approved by the Australian Therapeutic Goods Administration (TGA).
April 2020
Partnership with HK Winhealth Pharma Group Co. Limited in China announced.
October 2019
US Food and Drug Administration grant marketing approval for SCENESSE®.
December 2014
SCENESSE® (afamelanotide 16mg) approved by European Medicines Agency (EMA).
References
Langendonk JG, Balwani M, Anderson KE, Bonkovsky HL, Anstey AV, Bissell DM, Bloomer J, Edwards C, Neumann NJ, Parker C, Phillips JD. Afamelanotide for erythropoietic protoporphyria. New England Journal of Medicine. 2015 Jul 2;373(1):48-59.
Harms J, Lautenschlager S, Minder CE, Minder EI. An α-melanocyte–stimulating hormone analogue in erythropoietic protoporphyria. New England Journal of Medicine. 2009;360(3):306-307.
Murphy GM. Diagnosis and management of the erythropoietic porphyrias. Dermatol Ther. 2003;16(1):57-64.
Thunell S, Harper P, Brun A. Porphyrins, porphyrin metabolism and porphyrias. IV. Pathophysiology of erythyropoietic protoporphyria–diagnosis, care and monitoring of the patient. Scand J Clin Lab Invest. 2000;60(7):581-604.
Todd DJ. Clinical implications of the molecular biology of erythropoietic protoporphyria. Journal of the European Academy of Dermatology and Venereology. 1998 Nov;11(3):207-13.