SCENESSE® in DNA Repair
CLINUVEL to confirm cellular DNA repair in rare disease xeroderma pigmentosum (XP)
A separate media release – in simple non-technical terms – has been lodged outlining the aims and objectives of the DNA Repair Program. CLINUVEL will post background information on XP to its social media channels:
Twitter | Facebook | Instagram | LinkedIn
EXECUTIVE SUMMARY
- CLINUVEL to confirm in clinical trials the role of SCENESSE® in cellular UV-induced DNA repair
- XP is a rare genetic life-threatening and mutilating disorder making patients susceptible to 10,000-fold
risk of skin cancers throughout their lives (median survival of 30 years – prevalence 1:450,000) - Clinical objectives for SCENESSE®:
1. systemic photoprotection to skin cells;
2. optimisation of the response of skin cells to UV radiation;
3. anti-oxidative capacity;
4. elimination of photoproducts (chemical damage to DNA);
5. increased activity of DNA repair genes (as part of NER and/or BER); and
6. reduction of cell death (apoptosis) following UV exposure.
CLINUVEL (UK) LTD, a wholly owned subsidiary of CLINUVEL PHARMACEUTICALS LTD, today announced it is evaluating SCENESSE® (afamelanotide 16mg) in patients with the rare disorder xeroderma pigmentosum (XP)1 to progress its novel DNA Repair Development Program. 1 SCENESSE® is understood to protect and repair DNA, a
concept that will now be confirmed in the clinic.
DNA DAMAGE AND REPAIR
Ultraviolet (UVB of wavelengths 290-320 nm and UVA of 320-400 nm) and high energy visible (HEV, 400-600 nm) light penetrate human skin leading to cellular oxidative stress and damage to DNA within the nucleus of skin cells. This damage consists of changes to the DNA structure (photoproducts) 2 which, if left unrepaired, can replicate and increase the risk of skin cancers, such as melanoma.
Under normal conditions, human biology is capable of repairing DNA damage through nucleotide excision repair and/or base excision repair (NER and BER, respectively), in which defective strands of DNA are “snipped” and removed, and replaced by the correct DNA sequences. XP patients, organ transplant recipients and people of AngloSaxon origin with red hair, blue eyes and fair skin are at the highest risk of developing skin cancers because they have either insufficient or defective NER and BER, i.e. a reduced capacity to repair damaged DNA.
STAGED DEVELOPMENT PROGRAM: SCENESSE® IN DNA DAMAGE REPAIR
Scientific evidence supports the use of afamelanotide, the active ingredient in SCENESSE®, for photoprotection and repair of UV-induced DNA damage.
During the development of SCENESSE®, a number of categories of scientific evidence have been accumulated:
- systemic photoprotection to skin cells;
- optimisation of the response of skin cells to UV radiation;
- anti-oxidative capacity;
- elimination of photoproducts (chemical damage to DNA);
- increased activity of DNA repair genes (as part of NER and/or BER); and
- reduction of cell death (apoptosis) following UV exposure.
- CLINUVEL to confirm in clinical trials the role of SCENESSE® in cellular UV-induced DNA repair
- XP is a rare genetic life-threatening and mutilating disorder making patients susceptible to 10,000-fold
risk of skin cancers throughout their lives (median survival of 30 years – prevalence 1:450,000) - Clinical objectives for SCENESSE®:
1. systemic photoprotection to skin cells;
2. optimisation of the response of skin cells to UV radiation;
3. anti-oxidative capacity;
4. elimination of photoproducts (chemical damage to DNA);
5. increased activity of DNA repair genes (as part of NER and/or BER); and
6. reduction of cell death (apoptosis) following UV exposure.
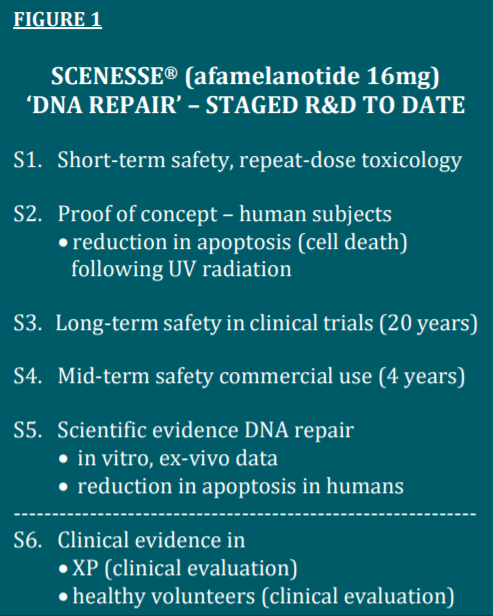
Figure 1 illustrates how the DNA Repair Program has placed emphasis on the safety of patients and volunteers exposed to afamelanotide – more than 10,000 doses in over 1,400 subjects – during 20 years of clinical use, a requisite to being able to complete the clinical use of the hormone as a DNA restorative drug in patients at the highest risk of contracting skin cancers.
Stages S1 to S5 have been evaluated by the Company and regulatory authorities as satisfactory and complete, enabling Stage 6 of clinical investigation in the scope of SCENESSE® as a DNA-regenerative pharmaceutical therapy. Clinical stage S6
consists first of a Special Access Program in XP to confirm the safety of the drug in this highest-risk population, followed by a pilot study in XP-C (CUV150), and a parallel control study in healthy volunteers (CUV151) who are exposed to UV radiation
under standardised conditions.
The exact biochemical and cellular mechanisms of UV-induced cellular damage and repair by SCENESSE® are explained in technical terms in Figure 2, attached below.
XERODERMA PIGMENTOSUM
XP is a group of disorders expressing eight different genes (XPA to G, and V) involved in the NER process, with a collective prevalence of approximately 1:450,000 in the European population. Due to these genetic deficiencies in DNA repair proteins, XP patients are 10,000-fold more susceptible to skin cancers including melanoma, necessitating them to shield from ambient and outdoor light from birth onwards.
The consequences of exposure to non-ionising radiation (UV) are severe as many XP patients suffer loss of extremities, facial anatomy such as ears, and eye-sight due to the lack of fully functional DNA repair. The median age of survival for XP patients is approximately 30 years.
SCENESSE® will first be evaluated in XP-C patients – carrying a defect in gene 3p25.1 – since it is the most prevalent form of XP in Europe and the United States. XP-C is characterised by an insufficiency of the damage recognition protein XP-C required for efficient DNA repair of skin cells.
CLINUVEL will publish when the first XP-C patient has been administered with SCENESSE®.
COMMENTARY
“We are delighted to be able to proceed with the landmark evaluation of SCENESSE® in XP and putting the final piece of evidence together for the melanocortin product as a DNA-regenerative pharmaceutical solution,” CLINUVEL’s Chief Scientific Officer, Dr Dennis Wright said.
“Worldwide, there is no therapy available in XP and we are compelled to help these patients since they lead a compromised and short life. “The clinical challenge is enormous as we aim to confirm defined effects from SCENESSE® in XP patients which will need to lead to the conclusion that DNA regeneration is assisted and accelerated. I can only applaud our team who have been remarkably patient, working over many years to meet regulatory and ethics requirements,” Dr Wright said.
“As we progress through the two clinical studies we will be evaluating available assays needed to validate positive effects on DNA repair in XP patients,” CLINUVEL’s Clinical Operations Manager, Dr Pilar Bilbao said. “It is an exciting time as we are already starting from a positive base knowing that SCENESSE® reduces apoptotic cells following UV exposure; now the next objective is to demonstrate this very effect in XP patients.
“We expect the first results in 2021 and will monitor the safety of the XP patients receiving SCENESSE® day to day. It is of high relevance to confirm the role of SCENESSE® in UV radiation damage regeneration and will improve the general understanding how to reduce skin cancer risk for many of us” Dr Bilbao said.
1 SCENESSE® (afamelanotide 16mg) is approved in the European Union as an orphan medicinal product for the prevention of phototoxicity in adult patients with erythropoietic protoporphyria (EPP). SCENESSE® is approved in the USA to increase “painfree” light exposure in adult EPP patients with a history of phototoxicity. Information on the product can be found on CLINUVEL’s website at www.clinuvel.com. 2 Cyclobutane pyrimidine dimers (CPDs), 6-4 pyrimidine pyrimidone dimers (6-4 PPs) and Dewars isomers are formed within seconds of exposure of unprotected skin to radiation, causing breaks in the strands of DNA.
Download Pdf